Practice Management
Practice Management
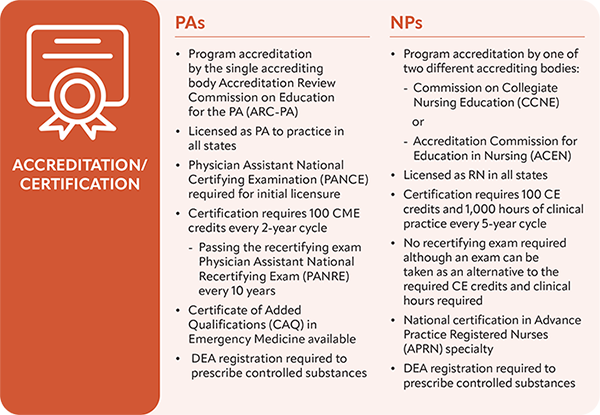
Emergency medicine physician assistants (EMPAs) have been providing quality and compassionate care to patients for more than 50 years. In that time, PAs continue to be educated and trained through intensive programs that maintain rigorous teaching standards. Over the last few years, physician organizations have been circulating narratives that aim to disparage EMPA education and training and undermine the EMPA profession. Additionally, these narratives typically link nurse practitioners (NPs) with PAs despite the fact that PAs and NPs have different education and training models and standards. As the national organization for EMPAs that has always supported and advocated for the ongoing education and training of EMPAs, the Society of Emergency Medicine Physician Assistants (SEMPA) is providing accurate and clear information regarding EMPA education, training and credentialing, and how it compares to that of NPs in order to address the unfounded narratives.
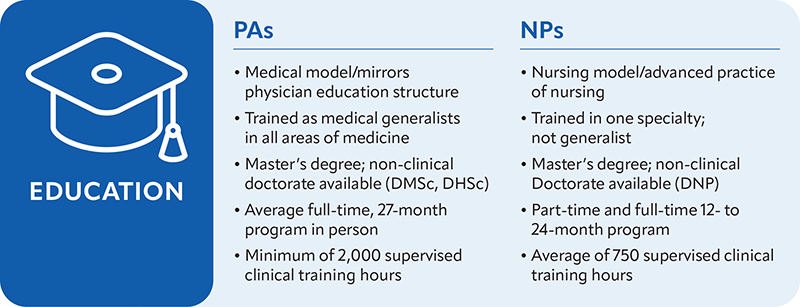
Recent data shows that EMPAs – with appropriate training and oversight in a team-based practice – provide safe, high-quality, evidence-based patient care in all emergency departments settings (1) Pines 2020, (2) Wu 2021. There are unique aspects of EMPA education and training that warrant highlighting when compared to the education and training of NPs.
Most EMPAs accumulate thousands of direct patient care hours in various health care roles prior to being accepted into PA school. The focus of PA education is to provide a foundation of general medicine practice, which mirrors the physician training model. All PAs complete at least 4,000 hours of rigorous didactic and clinical training in general medicine that includes supervised clinical rotations in multiple specialties. After PA school, EMPAs acquire additional emergency medicine specific knowledge and experience via two pathways. Approximately 10% of all EMPAs complete additional formal postgraduate training in emergency medicine, which includes 2,000 to 3,000 hours of competency-based training supervised directly by emergency medicine physicians in addition to rigorous required didactic components (3). Alternatively, most EMPAs still train in the traditional physician mentorship model over the first several years of practice. This physician mentorship model – a notable difference between PA and NP training – is the foundation of PA training and a critical piece of information often not described or acknowledged in many statements made by physician organizations. EMPAs value and rely on the relationships with emergency physicians to gain knowledge and skills to be prepared to manage patients of any acuity level in the emergency department.
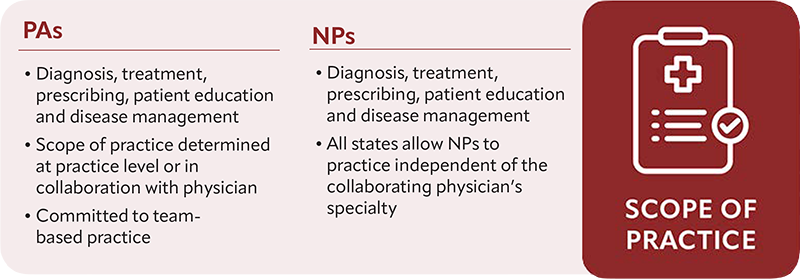
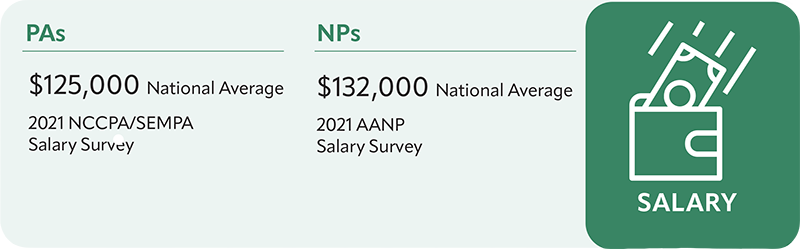
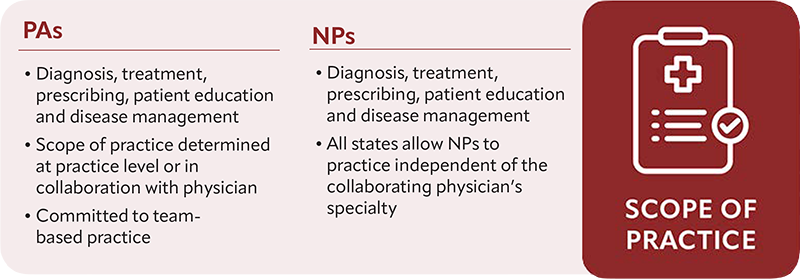
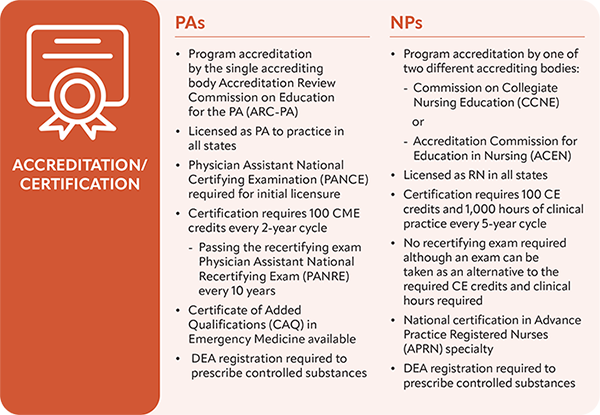
Despite these clear differences in education, PAs and NPs are commonly thought of as interchangeable regarding their roles and qualifications. While PAs and NPs are both integral to emergency medicine and in the care given in the emergency department, the professions are distinct and have unique differences. To group the two together using general terms such as advanced practice provider (APP), midlevel provider (MLP), and nonphysician provider (NPP), is a disservice to both professions and causes confusion.
In January 2020, SEMPA issued a policy statement on the use of these combined terms stating that they should be avoided (4). Rather, to accurately identify these professions and avoid confusion among the public and other organizations, EMPAs and NPs can simply be identified by these individual professional titles. Both the PA and NP professions come from very different but rich historical roots and have evolved to be uniquely adaptable in the modern complex health care system.
References
- Pines JM, Zocchi MS, Ritsema T, Polansky M, Bedolla J, Venkat A; US Acute Care Solutions Research Group. The Impact of Advanced Practice Provider Staffing on Emergency Department Care: Productivity, Flow, Safety, and Experience. Acad Emerg Med. 2020 Nov;27(11):1089-1099. doi: 10.1111/acem.14077. Epub 2020 Jul 31. PMID: 32638486.
- F, Weinstock M, Darracq M. Physician Assistant Malpractice Trends in Emergency Medicine. Ann Emerg Med. 2021 Oct; 78 (4): S7. https://doi: 10.1016/j.annemergmed.2021.09.023.
- https://www.nccpa.net/wp-content/uploads/2022/05/Emergency-Medicine-PAs-NCCPA-SEMPA-Survey-Report-Final-05.10.22.pdf
- https://sempa.org/siteassets/sempa/media/pdf/about-sempa/title-of-physician-assistant-policy-statement---final-january-28-2020.pdf
Practice Management
Practice Management
Emergency medicine physician assistants (EMPAs) have been providing quality and compassionate care to patients for more than 50 years. In that time, PAs continue to be educated and trained through intensive programs that maintain rigorous teaching standards. Over the last few years, physician organizations have been circulating narratives that aim to disparage EMPA education and training and undermine the EMPA profession. Additionally, these narratives typically link nurse practitioners (NPs) with PAs despite the fact that PAs and NPs have different education and training models and standards. As the national organization for EMPAs that has always supported and advocated for the ongoing education and training of EMPAs, the Society of Emergency Medicine Physician Assistants (SEMPA) is providing accurate and clear information regarding EMPA education, training and credentialing, and how it compares to that of NPs in order to address the unfounded narratives.
Recent data shows that EMPAs – with appropriate training and oversight in a team-based practice – provide safe, high-quality, evidence-based patient care in all emergency departments settings (1) Pines 2020, (2) Wu 2021. There are unique aspects of EMPA education and training that warrant highlighting when compared to the education and training of NPs.
Most EMPAs accumulate thousands of direct patient care hours in various health care roles prior to being accepted into PA school. The focus of PA education is to provide a foundation of general medicine practice, which mirrors the physician training model. All PAs complete at least 4,000 hours of rigorous didactic and clinical training in general medicine that includes supervised clinical rotations in multiple specialties. After PA school, EMPAs acquire additional emergency medicine specific knowledge and experience via two pathways. Approximately 10% of all EMPAs complete additional formal postgraduate training in emergency medicine, which includes 2,000 to 3,000 hours of competency-based training supervised directly by emergency medicine physicians in addition to rigorous required didactic components (3). Alternatively, most EMPAs still train in the traditional physician mentorship model over the first several years of practice. This physician mentorship model – a notable difference between PA and NP training – is the foundation of PA training and a critical piece of information often not described or acknowledged in many statements made by physician organizations. EMPAs value and rely on the relationships with emergency physicians to gain knowledge and skills to be prepared to manage patients of any acuity level in the emergency department.
Despite these clear differences in education, PAs and NPs are commonly thought of as interchangeable regarding their roles and qualifications. While PAs and NPs are both integral to emergency medicine and in the care given in the emergency department, the professions are distinct and have unique differences. To group the two together using general terms such as advanced practice provider (APP), midlevel provider (MLP), and nonphysician provider (NPP), is a disservice to both professions and causes confusion.
In January 2020, SEMPA issued a policy statement on the use of these combined terms stating that they should be avoided (4). Rather, to accurately identify these professions and avoid confusion among the public and other organizations, EMPAs and NPs can simply be identified by these individual professional titles. Both the PA and NP professions come from very different but rich historical roots and have evolved to be uniquely adaptable in the modern complex health care system.
References
- Pines JM, Zocchi MS, Ritsema T, Polansky M, Bedolla J, Venkat A; US Acute Care Solutions Research Group. The Impact of Advanced Practice Provider Staffing on Emergency Department Care: Productivity, Flow, Safety, and Experience. Acad Emerg Med. 2020 Nov;27(11):1089-1099. doi: 10.1111/acem.14077. Epub 2020 Jul 31. PMID: 32638486.
- F, Weinstock M, Darracq M. Physician Assistant Malpractice Trends in Emergency Medicine. Ann Emerg Med. 2021 Oct; 78 (4): S7. https://doi: 10.1016/j.annemergmed.2021.09.023.
- https://www.nccpa.net/wp-content/uploads/2022/05/Emergency-Medicine-PAs-NCCPA-SEMPA-Survey-Report-Final-05.10.22.pdf
- https://sempa.org/siteassets/sempa/media/pdf/about-sempa/title-of-physician-assistant-policy-statement---final-january-28-2020.pdf